Prominent ears can sometimes be called “Bat ears” “lop ears” or “protruding ears”. They can run in families, but do not cause any problems with hearing.
They are often the cause of teasing and bullying in childhood and this can carry on into adult life reducing confidence and psychological well-being.
Prominent ears may be unilateral (one-sided) or bilateral (both sided). Otoplasty or Pinnaplasty describes the operation to make the ears less prominent.
The Cause Of Prominent Ears
The parts of the ear that make it appear more prominent are a loss of the fold of the ear called the anti-helical fold, a deep enlarged bowl of the ear (conchal bowl) and earlobes that may stick out or appear too large.
While prominent ears do not usually cause physical discomfort, hearing loss or reduce the efficiency of the ear at all, they often cause psychological distress and affect self-esteem. The age at which our patients request a consultation for prominent ears varies. Rest assured that Mark can correct prominent ears while the patient is a child, or in adulthood.
Before Considering Corrective Surgery
There are several ways to correct prominent ears and the precise method will be case dependent. Before undergoing any type of otoplasty procedure, you should consider the following:
- Why do I want an Otoplasty?
- What do I expect of Otoplasty surgery?
- Am I prepared for the expense?
Despite surgical skill, expertise and the very best of care, results cannot be guaranteed and there are risks to consider.
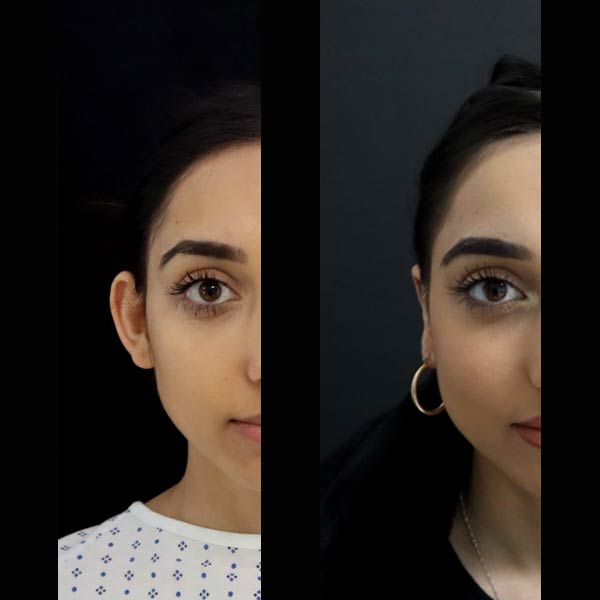
Hover Over Image To See Result


Hover Over Image To See Result


You should have realistic expectations as it isn’t possible to guarantee perfect results. A number of factors will be taken into account in your assessment for otoplasty surgery, such as; your age, skin texture, your own anatomy, healing properties and your general health. Any of these factors can influence the outcome of your surgery.
The Procedure
Otoplasty (Open Access Technique)
The commonest otoplasty technique used is to make an incision behind the ear and remove a thin strip of skin to gain access to the cartilage of the ear.
Next, permanent sutures are then placed into the cartilage of the ear which fold it back correcting the prominence.
This technique may be combined with one or more extra procedures in order to achieve the desired appearance of the client.
A less common technique is to create scratches in the front surface of the cartilage which soften it and cause it to fold backwards reducing the prominence. This is called the anterior scoring technique.
Otoplasty Plus Conchal Bowl Reduction
This involves the technique described above but may also involve reducing the depth of the bowl of the ear by removing a thin strip of cartilage. This makes the lower part of the ear less prominent.
Otoplasty Plus Ear Lobe Correction
The earlobes may also be prominent and either repositioning or reducing the earlobes in size as and additional procedure with the standard otoplasty.
Otopexy
Otopexy or Auropexy describes moving an ear to a higher position on the side of the head. It involves placing stitches that lift the ear up and is done through the same incision as an otoplasty.
Why Choose Mark Sheldon Lloyd For Your Otoplasty
As one of the few ear-reconstruction surgeons in the UK, Mark has a great deal of experience of treating all types of ear shapes and sizes. This experience has enabled him to hone his skills, handling cartilage and skin with the utmost care. With the finesse that experience, confidence and care brings, he is able to optimise each procedure to deliver the best aesthetic outcome.
About Otoplasty Procedure & Risks
Your Outpatient Visit
Otoplasty is performed as a day case in a high-quality state of the art operating theatre with trained nursing staff present.
After a standard open otoplasty, a light, padded dressing is placed behind the ears, to absorb any fluid that may appear from the wound in the first day or so. Occasionally a light head bandage is used to cover the ears, however, this does not need to be worn for more than a day.
At night, it is a headband – such as those that tennis players wear – is worn over the tops of the ears to stop them curling over on the pillow.
Typical Duration Of Surgery
The Otoplasty procedures take around two hours. Surgery may take longer if additional procedures are also required.
Recovery / Healing Time
Open otoplasty causes minimal bruising, but there may be a little leakage of fluid from the wounds in the first day or so prior to everything settling down.
Type Of Anaesthesia Required
Otoplasty can be done by making the ears numb with small injections that are given around the ear. The first injection is slightly uncomfortable but quickly become comfortable as the anaesthetic starts to make the skin numb.
Risks Associated With Otoplasty
Short Term Effects
You are likely to have swelling with hardness and bruising following surgery and in the immediate post-operative recovery period.
Twinges of pain may continue for the first few weeks following surgery, If you do experience severe or increasing pain, contact your clinic nurse on the advised out of hours contact number
Risks & Conditions
- Bleeding (haematoma). Occasionally, after surgery, blood may pool under the skin (haematoma) and should disperse spontaneously over 2 to 3 weeks. Occasionally, it needs to be drained surgically if larger and fails to disperse. In a standard open otoplasty, the haematoma forms behind the ear.
- In a very small number of patients, fluid that has not escaped may form a pocket (this is known as a seroma). Additional treatment may be needed to remove this fluid.
- It is important to recognise that a surgical incision or the introduction into the body of any foreign material contributes to a risk of the introduction of bacteria from the patient’s own skin. Such infection may be associated with tiredness, weakness, fever and muscle aches and pains. Antibiotics are not normally given during Otoplasty and there is no evidence that by giving antibiotics the chance of an infection occurring will be reduced. Rarely, a patient may require readmission to the hospital. If you experience any symptoms of infection, contact your clinic nurse or the advised out of hours contact number.
- Wound healing. Healing of wounds varies from patient to patient and even from one part of the body to another and is a gradual process. Smoking for the period leading up to your surgery and afterwards can seriously hinder the healing process and can cause serious problems such as infection.
- Small cysts called milia can form along the scar line. This is normally temporary, but sometimes may need surgical removal.
- Scar variability and keloids. All prospective patients must be aware that the rate at which their scars may heal and fade are entirely variable and individual. Uncommonly, a scar does not heal in the normal way. This is known as hypertrophic scarring meaning the scar is excessively thick. Scars may be red, or highly coloured, thick, painful and may take several years to improve if at all. Although this an unusual problem, it cannot be avoided or diagnosed in advance. Scar location for standard open Pinnaplasty is behind the ear. Scars that overgrow in size are known as keloid scars. These occasionally need treatment but are not curable and remain for life to some degree.
- Otoplasty is not an exact science and healing is not a symmetrical process. There maybe a slight difference between the right and the left sides and this may be noticeable several months after the surgery when the swelling has gone down. Absolute symmetry cannot be guaranteed.
- Recurrence of prominent ears. Occasionally, the ears may become prominent again. This may be due to the sutures weakening over time, or the cartilage being too stiff to fold back.
- Deep Vein Thrombosis and Pulmonary Embolism. This is a rare but serious complication of surgery and general anaesthesia, where a blood clot forms in the veins, usually the legs, and then moves to the lungs interfering with their normal function. The incidence of DVT is 1:5000 cases. The medical and nursing staff take active measures to reduce the chance of this happening; you may be asked to wear special stockings during your admission and will be actively encouraged to mobilise early following surgery. You can further reduce the risks after discharge by avoiding dehydration and remaining mobile. If you experience sudden chest pain or breathlessness, you should seek medical help without delay. An exceptionally rare occurrence is a fat embolism, the symptoms of which are the same as a pulmonary embolism.
- As with any type of surgery, there is always a possibility that your surgeon is of the opinion that you could benefit from some form of revision operation after your original surgery and assessment of the final outcome of your primary surgery. Please refer to the Readmission Policy (within our booklet) for our terms and conditions.
- Patients must recognise that this procedure is performed for cosmetic reasons and because of this, the results can only be assessed subjectively. Therefore, it is important to understand that while you will be advised as to the probable results, this should in no way be interpreted as a guarantee for the outcome of surgery.
- Numbness or oversensitive skin. This can take several weeks to recover and can be helped by the skin over the ear being gently massaged so that the skin begins to have sensory re-education i.e. the skin knows how it should feel after surgery.
The list of risks and conditions associated with otoplasty is not exhaustive. It is important that patients recognise that it is not always possible for the surgeon to predetermine the individual and psychological reaction of patients to post-operative complications.